988 suicide crisis helpline launches across Canada
Improving mental health by training the suppression of unwanted thoughts
SPOTLIGHT ON WILDERNESS THERAPY: JUST “GET OUTSIDE”: THE O2 PROJECT

Canada's 988 hotline, which gives people access to suicide prevention services via call or text, went live on Thursday.
People in every province and territory who are experiencing a mental health crisis and need immediate, real-time support can use the three-digit number.
Similar to 911 for accessing fire, police and medical emergencies, 988: Suicide Crisis Helpline is a short, easy-to-remember number to get a quick response from coast to coast to coast, 24/7 and free of charge.
Read full article here:
https://www.cbc.ca/news/health/988-hotline-mental-health-canada-1.7043603
SPOTLIGHT ON WILDERNESS THERAPY: JUST “GET OUTSIDE”: THE O2 PROJECT
Improving mental health by training the suppression of unwanted thoughts
SPOTLIGHT ON WILDERNESS THERAPY: JUST “GET OUTSIDE”: THE O2 PROJECT

''As inspirational as Ben was, he also battled anxiety, depression, and alcohol addiction,” says the o2 website of Ben’s story. “Ben knew better than most how inner turmoil can devastate an otherwise extraordinary life.”
Pine River is extremely grateful to be a recipient of this fundraising, for three years running. This year’s grant is earmarked for Pine River’s Outdoor Leadership Experience (OLE) and is hugely welcome support!
Wilderness therapy is a core tenant of Pine River’s program for youth struggling with addiction and other mental health issues. All of our students start the first phase of our program “in the woods,” and throughout their time at Pine River, they participate in re-grounding and mentorship for new students, while also spending time in canoes, hiking and daily outdoors in nature throughout the program.
Our OLE has students in the wilderness 24 hours/day, 365 days/year.
Read full article here:
https://pineriverinstitute.com/news/spotlight-on-wilderness-therapy-just-get-outside-the-o2-project/
Improving mental health by training the suppression of unwanted thoughts
Improving mental health by training the suppression of unwanted thoughts
Improving mental health by training the suppression of unwanted thoughts
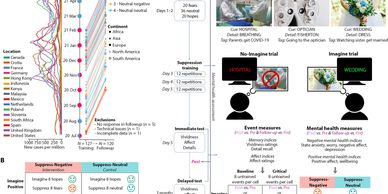
Anxiety, posttraumatic stress, and depression markedly increased worldwide during the COVID-19 pandemic. People with these conditions experience distressing intrusive thoughts, yet conventional therapies often urge them to avoid suppressing their thoughts because intrusions might rebound in intensity and frequency, worsening the disorders. In contrast, we hypothesized that training thought suppression would improve mental health. One hundred and twenty adults from 16 countries underwent 3 days of online training to suppress either fearful or neutral thoughts. No paradoxical increases in fears occurred. Instead, suppression reduced memory for suppressed fears and rendered them less vivid and anxiety provoking.
Read full article here:
What is mental health?
Young people’s mental health is finally getting the attention it needs
Improving mental health by training the suppression of unwanted thoughts

Mental health is all about how people think, feel, and behave. Mental health specialists can help people with depression, anxiety, bipolar disorder, addiction, and other conditions that affect their thoughts, feelings, and behaviors.
Mental health can affect daily living, relationships, and physical health.
However, this link also works in the other direction. Factors in people’s lives, interpersonal connections, and physical factors can contribute to mental ill health.
Looking after mental health can preserve a person’s ability to enjoy life. Doing this involves balancing life activities, responsibilities, and efforts to achieve psychological resilience.
Read full article here:
Mental Health
Young people’s mental health is finally getting the attention it needs
Young people’s mental health is finally getting the attention it needs

Everyone feels worried or anxious or down from time to time. But relatively few people develop a mental illness. What's the difference? A mental illness is a mental health condition that gets in the way of thinking, relating to others, and day-to-day function.
Dozens of mental illnesses have been identified and defined. They include depression, generalized anxiety disorder, bipolar disorder, obsessive-compulsive disorder, post-traumatic stress disorder, schizophrenia, and many more.
Mental illness is an equal opportunity issue. It affects young and old, male and female, and individuals of every race, ethnic background, education level, and income level. The good news is that it can often be treated.
Read full article here:
Young people’s mental health is finally getting the attention it needs
Young people’s mental health is finally getting the attention it needs
Young people’s mental health is finally getting the attention it needs

Worldwide, at least 13% of people between the ages of 10 and 19 live with a diagnosed mental-health disorder, according to the latest State of the World’s Children report, published this week by the United Nations children’s charity UNICEF. It’s the first time in the organization’s history that this flagship report has tackled the challenges in and opportunities for preventing and treating mental-health problems among young people. It reveals that adolescent mental health is highly complex, understudied — and underfunded. These findings are echoed in a parallel collection of review articles published this week in a number of Springer Nature journals.
Read full article here:
USA -New 988 mental health crisis line sees ‘eye-opening’ rise in calls, texts, chats in first 6 mon
USA -New 988 mental health crisis line sees ‘eye-opening’ rise in calls, texts, chats in first 6 mon
USA -New 988 mental health crisis line sees ‘eye-opening’ rise in calls, texts, chats in first 6 mon

We know that there are many individuals in this country who are struggling with suicidal concerns, with mental health or substance use concerns, who aren’t able to access the care that they need. And in many respects, historically, because of funding limitations or other limitations, the system has let them down,” Palmieri said. “So, this is truly an opportunity with 988 – as a catalytic moment – to be able to transform the crisis care system to better meet those needs in a less restrictive, more person-centered, more treatment- and recovery-oriented way.”
Read full article here:
https://www.cnn.com/2023/01/19/health/988-lifeline-first-six-months-cnn-analysis/index.html
It’s time to recognize mental health as essential to physical health
USA -New 988 mental health crisis line sees ‘eye-opening’ rise in calls, texts, chats in first 6 mon
USA -New 988 mental health crisis line sees ‘eye-opening’ rise in calls, texts, chats in first 6 mon

The human brain is a wonder. Through folds of tissue and pulses of electricity, it lets us perceive, attempt to understand, and shape the world around us. As science rapidly charts the brain’s complex structures, new discoveries are revealing the biology of how the mind functions and fails. Given the centrality of the brain to human health, its malfunctions should be a priority, separated from stigma and treated on par with the diseases of the body. We aren’t there yet, but the transformation is underway.
Mental disorders affect nearly 20 percent of American adults; nearly 4 percent are severely impaired and classified as having serious mental illness. These disorders are often associated with chronic physical illnesses such as heart disease and diabetes. They also increase the risk of physical injury and death through accidents, violence, and suicide.
Read full article here:
THE IMPORTANCE OF MENTAL HEALTH AWARENESS
USA -New 988 mental health crisis line sees ‘eye-opening’ rise in calls, texts, chats in first 6 mon
THE IMPORTANCE OF MENTAL HEALTH AWARENESS

Mental illnesses affect 19% of the adult population, 46% of teenagers and 13% of children each year. People struggling with their mental health may be in your family, live next door, teach your children, work in the next cubicle or sit in the same church pew.
However, only half of those affected receive treatment, often because of the stigma attached to mental health. Untreated, mental illness can contribute to higher medical expenses, poorer performance at school and work, fewer employment opportunities and increased risk of suicide.
Read full article here:
https://www.pinerest.org/newsroom/articles/mental-health-awareness-blog/
What is mental health?
Young people’s mental health is finally getting the attention it needs
THE IMPORTANCE OF MENTAL HEALTH AWARENESS

Mental health is all about how people think, feel, and behave. Mental health specialists can help people with depression, anxiety, bipolar disorder, addiction, and other conditions that affect their thoughts, feelings, and behaviors.
Mental health can affect daily living, relationships, and physical health.
However, this link also works in the other direction. Factors in people’s lives, interpersonal connections, and physical factors can contribute to mental ill health.
Looking after mental health can preserve a person’s ability to enjoy life. Doing this involves balancing life activities, responsibilities, and efforts to achieve psychological resilience.
Read full article here:
Mental Health
Young people’s mental health is finally getting the attention it needs
Young people’s mental health is finally getting the attention it needs

Everyone feels worried or anxious or down from time to time. But relatively few people develop a mental illness. What's the difference? A mental illness is a mental health condition that gets in the way of thinking, relating to others, and day-to-day function.
Dozens of mental illnesses have been identified and defined. They include depression, generalized anxiety disorder, bipolar disorder, obsessive-compulsive disorder, post-traumatic stress disorder, schizophrenia, and many more.
Mental illness is an equal opportunity issue. It affects young and old, male and female, and individuals of every race, ethnic background, education level, and income level. The good news is that it can often be treated.
Read full article here:
Young people’s mental health is finally getting the attention it needs
Young people’s mental health is finally getting the attention it needs
Young people’s mental health is finally getting the attention it needs

Worldwide, at least 13% of people between the ages of 10 and 19 live with a diagnosed mental-health disorder, according to the latest State of the World’s Children report, published this week by the United Nations children’s charity UNICEF. It’s the first time in the organization’s history that this flagship report has tackled the challenges in and opportunities for preventing and treating mental-health problems among young people. It reveals that adolescent mental health is highly complex, understudied — and underfunded. These findings are echoed in a parallel collection of review articles published this week in a number of Springer Nature journals.
Read full article here:

Prescribing nature: Research suggests the outdoors are good for your mental health
Dr. Melissa Lem says spending time outdoors can clear our minds, lower our stress.
For many teenagers, a driver's licence can mean freedom to visit the mall — but for Jon Cadang, it offered him a reprieve from the depression that consumed him for years.
One of his first stops? A creek near his home in Mississauga, Ont., abundant in fish that he was determined to catch.
It would take Cadang two weeks before he landed one, but it taught the forager and painter that nature could be a powerful treatment to what ails him.
"I realized that whole time, I stopped ruminating about my situation — all the bad things that were happening," said Cadang, now 25. "I realized that maybe being out here and putting myself towards a goal, even if that's just to catch fish, maybe that could help," he told Back to the Land host Duncan McCue.
"I liked what I saw. I felt at peace."
A growing body of research suggests that being outdoors can benefit mental health and boost memory, improve cardiovascular health and help us live longer. Additional studies find that nature lowers cortisol, the body's stress hormone.
With that research in hand, doctors in parts of Canada have signed on to provide what are known as "nature prescriptions" for those living with mental illnesses and physical health conditions such as heart disease and diabetes.
Read full article here:

Ontario To Provide Free Therapy For People With Anxiety Or Depression
“Through this ground-breaking program, an individual will receive an assessment from a trained mental health clinician and offered a therapy program that best addresses their level of need.”
Ontarians will soon be able to get free therapy for anxiety and depression through a program called Mindability, the health minister announced Tuesday.
“Mindability will be funded just like OHIP [Ontario Health Insurance Plan], with no out-of-pocket cost to patients,” Minister Christine Elliott said at a mental health centre in Whitby, Ont.
“Through this groundbreaking program, an individual will receive an assessment from a trained mental health clinician and offered a therapy program that best addresses their level of need.”
She said the program will offer cognitive behavioural therapy only for people who have anxiety or depression.
Read full article here:
Site Content
FAST FACTS ABOUT MENTAL HEALTH AND MENTAL ILLNESS by CAMH

Mental health and mental illness: what’s the difference?
- Mental health and mental illness are often used interchangeably, but they are not the same thing.
- “Mental health” is a concept similar to “physical health”: it refers to a state of well-being. Mental health includes our emotions, feelings of connection to others, our thoughts and feelings, and being able to manage life’s highs and lows.
- The presence or absence of a mental illness is not a predictor of mental health; someone without a mental illness could have poor mental health, just as a person with a mental illness could have excellent mental health.
- Problematic substance use is sometimes linked to poor mental health or mental illness; it can be a coping strategy for untreated trauma, pain, challenging thoughts or emotions, or other health symptoms.
Who is affected?
- Everyone has mental health and will experience challenges regarding their mental well-being, but not everyone will experience a mental illness.
- Mental illness indirectly affects all Canadians at some time either through their own experience, or that of a family member, friend or colleague.
- In any given year, 1 in 5 people in Canada will personally experience a mental health problem or illness.
- By age 40, about 50% of the population will have or have had a mental illness.
- Mental illness affects people of all ages, education, income levels, and cultures; however, systemic inequalities such as racism, poverty, homelessness, discrimination, colonial and gender-based violence, among others, can worsen mental health and symptoms of mental illness, especially if mental health supports are difficult to access.
- Major depression affects approximately 5.4% of the Canadian population, and anxiety disorders affect 4.6% of the population.[1]
- About 1% of Canadians will experience bipolar disorder (formerly called “manic depression”), and another 1% will experience schizophrenia.
- Eating disorders affect approximately 1 million Canadians – between 0.3-1% of the population. They impact women at a rate ten times that of men, and have the highest rate of mortality of any mental illness.[2]
- Substance use disorders affect approximately 6% of Canadians.[3]
- 4,012 Canadians died by suicide in 2019.[4]
- In Canada, suicide disproportionately impacts Indigenous peoples; the rate of suicide among First Nations is three times higher than among non-Indigenous Canadians, and nine times higher among Inuit.[5]
- The mortality rate due to suicide among men is three times the rate among women, but girls and young women are three times more likely than men to harm themselves and be hospitalized from self-harm.[6]
Read full article here:
